How to treat uterine endometrium. Causal factors of the disease. Features of treatment of chronic endometritis
home
Content Endometritis is an inflammatory disease that develops inside the uterus due to negative impact
various pathogens. The main reasons include the following factors: a decrease in the level of acidity in the vagina, as well as improper functioning of antibodies and immunoglobulin. Many women consult a doctor because they suspect endometritis. Only a gynecologist can tell you what kind of disease this is and how to properly treat such inflammation. If not treated in a timely manner, the infection spreads to the fallopian tubes and appendages.
In most cases, endometritis occurs in women who have reached reproductive age.
How does endometritis appear? Endometritis develops
due to a pathogenic infection and spreads to the lower parts of the genitourinary system.
The disease is acute or chronic. In pregnant girls, inflammation appears after gynecological manipulations that were not performed with sterile instruments.
Infection can get inside the endometrium after labor. The chronic course of the disease is caused by the gradual accumulation of tissue that remains after labor or mechanical abortion. It is important for women to take care of their health during the postpartum period because a large open wound forms inside the uterus due to placental rejection. Through it, various infections and pathogenic bacteria get inside.
In non-pregnant women, the chronic form of endometritis is associated with the development of infectious processes. These include chlamydia, tuberculosis and bacterial vaginosis. Inflammation will make itself felt by an increase in body temperature and general malaise.
Causes
The endometrium in the uterus has a two-layer structure - the basal and functional layers. Even with the slightest cracks, an inflammatory process develops. Pathogenic bacteria penetrate into the tissue, which leads to complications. After some time, inflammation appears. This is due to fragility and hypersensitivity
layer.
- The most common factors that lead to endometrial damage can be identified:
- inaccurate douching,
- labor activity,
- fallopian tube injury during examination,
- probing and curettage of the uterine cavity.
 Various infections can lead to the development of endometrial inflammation - these are chlamydia, tuberculous microbacteria, Escherichia coli, Proteus, Klebsiella, diphtheria bacillus, enterobacteria, mycoplasma, and group B streptococci.
Various infections can lead to the development of endometrial inflammation - these are chlamydia, tuberculous microbacteria, Escherichia coli, Proteus, Klebsiella, diphtheria bacillus, enterobacteria, mycoplasma, and group B streptococci.
We should also highlight the following most common causes of uterine endometrium:
- regular stressful situations which lead to decreased immunity;
- lack of vitamins and chronic poisoning;
- diseases of internal organs;
- frequent change of sexual partners;
- failure to comply with basic rules of intimate hygiene.
Symptoms
Patients with uterine endometritis experience severe pain in the lower abdomen, pain when urinating and profuse vaginal discharge with an unpleasant odor. Symptoms are related to bacteria and infections. There are two forms of endometritis.
- Spicy.
- Patients experience pronounced symptoms - general malaise, nagging pain and tingling.
Hidden.
- The symptoms are sluggish, so endometritis in the uterine cavity can be diagnosed with a thorough and comprehensive examination.
- The following main symptoms can be identified:
- pain in the lower abdomen, which is similar to menstruation;
- increased body temperature;
- fatigue and general malaise;
- chills;
- depression;
- spotting, red, purulent and brown vaginal discharge that has an unpleasant odor;
heavy or scanty menstruation; soreness and enlarged uterus. Only a qualified gynecologist can determine endometritis inside the uterus. If the body temperature is elevated for several days, this indicates the presence of an inflammatory process in the body.
Even if the symptoms are mild, you should immediately consult a doctor.
It is not recommended to lower body temperature on your own using medications.
At the initial stage of uterine endometritis, women experience spotting of a reddish hue. After a few days without treatment, they become purulent and turn brown. The disease gradually progresses, and the infection spreads through the fallopian tubes.
After infection, inflammation manifests itself after a few days, and in the chronic form, symptoms do not appear for a long time. It is for this reason that it is important to visit your gynecologist regularly. Signs and the symptoms described above are added to them, then you need to immediately contact medical care. Thanks to modern methods diagnostics can facilitate therapeutic treatment, eliminate inflammation and prevent serious complications.
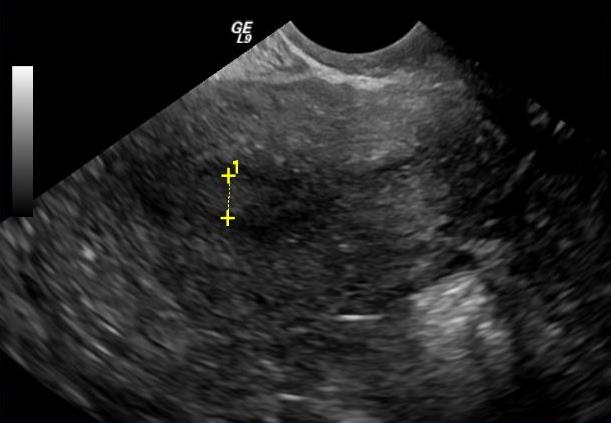
Indirect signs are determined by ultrasound examination. Only an experienced doctor will be able to distinguish between the symptoms of the initial and chronic forms of the disease. The echo sign of uterine endometritis can be determined by the following factors:
- degree of enlargement of the uterine cavity,
- thickness of formation,
- presence and number of adhesions.
Make an accurate diagnosis it is possible after a thorough study of the patient’s complaints, analysis of the regularity menstrual cycle and comprehensive examination.
When signs of endometritis on an ultrasound examination do not provide a detailed clinical picture of the severity and form of development, then material for a biopsy must be taken from the woman.
This is a rather complex and painful procedure, which is distinguished by its informative content. Such analysis should be carried out only in extreme dire situations. In the absence of the correct treatment regimen, inflammation develops into a more severe form, so the pathology often leads to infertility. It is important to completely treat endometritis inside the uterus and not let it progress, so that the inflammation does not become chronic and also does not infect other important organs.
Diagnostics
First stage Diagnosis of endometritis in the uterine cavity is a thorough examination of the patient and determination of symptoms. At the initial stage, a gynecological examination and palpation will help determine inflammation. If endometritis is suspected, the doctor will take a smear and material for culture.
Such laboratory tests will help determine the type and characteristics of the pathogen, as well as a possible response to drug treatment. If necessary, clinical and biochemical blood tests are prescribed. Experts will discover possible deviations leukocyte formula, acceleration of ESR and leukocyte level.
An effective method for diagnosing endometritis is an ultrasound examination of the uterus. The doctor evaluates the thickness of the mucous membrane, the presence of purulent formations, blood clots, remnants of placental tissue, inflammation, and changes in echogenic mucous membranes.
If treatment is untimely and incorrect, patients may experience the following complications:
- adhesive process,
- endometriosis,
- infection of newborns,
- complications during pregnancy,
- HIV infection,
- infertility,
- ectopic pregnancy,
- polyp on the cervix and erosion,
- menstrual irregularities.
Features of prevention
To avoid the development of uterine endometritis, it is important to exclude possible infection bacteria and viruses. To do this, you need to follow basic rules of personal hygiene. For any surgical intervention, women are prescribed special medications that have an antibacterial effect.
After an abortion and curettage in women, it is necessary to do an ultrasound of the uterine cavity to ensure complete removal all blood clots, remnants of the placenta or fertilized egg. Prevention of uterine endometritis - maintaining a healthy lifestyle and proper nutrition. With frequent changes of sexual partners, women may become infected, resulting in infection. In winter and autumn, you need to take vitamin complexes.
The disease endometritis occurs more often after childbirth, abortion, and intrauterine interventions. Symptoms of endometritis: increased body temperature to 38-39 ° C with endometritis; the appearance of serous, serous-purulent and bloody-purulent discharge from the genital tract is a particularly important symptom of endometritis, coupled with anamnesis and general malaise, which makes it possible to differentiate endometritis from inflammatory lesions of the lower genital tract (bacterial vaginosis, colpitis, etc.); the appearance of pain in the lower abdomen due to endometritis, radiating to the sacrum and general malaise.
Endometritis is an inflammatory disease of the uterine mucosa. When the muscular layer of the uterus is involved in the process, a diagnosis of metroendometritis is made.
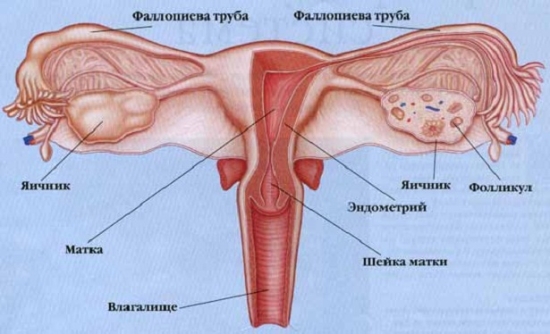
The uterus is structured like this: the cervix, the body of the uterus and two fallopian tubes. The body of the uterus is made up of the endometrium (the mucous membrane of the uterus - it is the rejection of the endometrium that is accompanied by bleeding during menstruation, the fertilized egg is also attached there), myometrium (the muscular lining of the uterus, which is stretchable during pregnancy ) and perimetry (the outer, serous membrane is a continuation of the peritoneum of the bladder). The endometrium and myometrium are histologically connected and pathological processes flow from one to the other layer.
The endometrium consists of two fundamentally different layers: the functional one - the one that exfoliates at the end of each menstruation and the basal one, which causes the formation of a new functional layer, and, therefore, determines the onset of the next menstruation. The functional layer is represented by one layer of cells, shaped like cylinders (cylindrical epithelium), between which are located glandular cells (produce the necessary mucus) and the terminal branches of small spiral arteries, which are located in large numbers here. Similar structure, single layer of cells and presence large number small vessels, is quite fragile and susceptible to adverse effects.
It is damage to the above structures that leads to the possibility of infection and the occurrence of an inflammatory process - endometritis. The close connection of all layers of the uterus and the absence of protective barriers between them leads to the transition of endometritis to metroendometritis.
Causes of endometritis
The main cause of endometritis is damage to the uterine mucosa, leading to the development of an inflammatory process. We must also understand that simple damage cannot lead to serious complications. Only the presence of reduced immunity, existing low-grade inflammation and non-compliance sanitary standards during manipulation can lead to inflammatory changes. The causes of damage may primarily be:
1. Curettage of the uterine cavity (medical abortion, curettage for bleeding and suspected cancer)
2. Probing of the uterine cavity
3. Hysterosalpingography (examination of the uterus and fallopian tubes, most often for the purpose of “blowing” in the treatment of infertility)
4. Hysteroscopy (endoscopic examination of the uterine cavity)
5. Placement of intrauterine contraceptives
6. Inaccurate douching
A special place is occupied by postpartum endometritis; they are primarily caused by a significant decrease and restructuring of the woman’s immune system. As a rule, endometritis spreads quite quickly to the muscle layer and is a serious complication of the postpartum period.
Endometritis is a polyetiological disease - caused by a group of pathogens, with the possible predominance of one. The most common causative agents of endometritis are:
1. Group B streptococci
2. Escherichia coli
3. Klebsiella
4. Enterobacter
5. Proteus
6. Chlamydia
7. Mycoplasmas
8. Diphtheria bacillus
9. Mycobacterium tuberculosis
In addition, viruses and protozoan microorganisms can also serve as pathogens.
Causes of chronic endometritis
The development of chronic endometritis is associated with inadequate treatment of acute endometritis or with an undiagnosed process, in which the infection exists in the tissues for a long time. The causative agent can be all of the above.
Symptoms of endometritis
Symptoms of endometritis are sometimes not clearly expressed, and the woman, unfortunately, does not pay attention to them, which subsequently leads to more severe inflammation of not only the mucous membrane, but also the muscular layer of the uterus, requiring hospitalization and inpatient treatment. Consequently, minimal knowledge of the signs of endometritis and the causes of its occurrence, timely contact with a doctor with these symptoms can prevent its transition to metroendometritis and allow doctors to significantly improve the quality of life of their patients.
Endometritis can be acute or chronic. If the treatment and diagnosis of acute endometritis, as a rule, does not present much difficulty, then the chronicity of the process causes many difficulties, both in diagnosis and in treatment. This is another reason why you should immediately consult a doctor at the first symptoms of endometritis.
Symptoms of acute endometritis
Most often, endometritis occurs after artificial termination of pregnancy. It goes without saying that criminal abortion in most cases leads to a similar complication due to the almost complete lack of compliance with sanitary standards. The disease begins with:
1. increase in body temperature to 38-39° C;
2. the appearance of serous, serous-purulent and bloody-purulent discharge from the genital tract - a particularly important symptom, coupled with anamnesis and general malaise, which makes it possible to differentiate endometritis from inflammatory lesions of the lower genital tract (bacterial vaginosis, colpitis, etc.);
3. the appearance of pain in the lower abdomen, radiating to the sacrum
4. general malaise.
IN similar situation You shouldn’t wait for everything to go away on its own and self-medicate - endometritis is an inflammatory disease, and any inflammatory disease tends to spread far from the location of the primary focus. Any self-medication in this situation, postponing a visit to an obstetrician-gynecologist leads to an inevitable increase in the risk of severe purulent-septic complications requiring long-term hospital treatment, which may well result in amputation of the uterus and the spread of infection - sepsis, with further death. Consequently, when the first symptoms appear, a woman who has recently given birth has undergone an artificial abortion operation, or some other invasive diagnostic procedure You should immediately consult a doctor and undergo a detailed examination.
It is necessary to clarify that we can talk about endometritis only if there are prerequisites for this - in the past there were some processes that affected the integrity of the uterine mucosa. In the absence of such, it is inappropriate to talk about endometritis if uncharacteristic discharge, pain or any other symptoms appear.
Symptoms of chronic endometritis
For chronic endometritis, it is difficult to identify symptoms that differ from acute form. The symptoms, in this case, are “fuzzy”. TO characteristic symptoms chronic endometritis can be attributed to:
1. Constantly lasting temperature for a long time.
2. Irregular uterine bleeding. Intermenstrual bleeding is associated with increased endometrial vascular permeability during ovulation. This change in blood vessels is also observed in healthy women, but blood cells are not visible in the discharge. The reasons causing uterine bleeding include a decrease in the contractile activity of the uterus and a violation of the aggregation properties of platelets.
3. The presence of constant discharge from the external genital tract, often of a putrefactive nature.
4. Pain during bowel movements.
Chronic endometritis does not prevent conception, which occurs in the presence of ovulation. In combination with concomitant ovarian dysfunction or other genital diseases, chronic endometritis causes reproductive dysfunction - infertility and spontaneous miscarriages, including habitual ones.
Diagnosis of endometritis
When contacting a doctor, you should tell him in detail your entire medical history and all the symptoms that led you to him, since already at this stage it becomes possible to assume that the patient has endometritis. In addition to your medical history, the doctor must:
1. will subject you to a gynecological examination in the speculum and palpation of the uterus - as a rule, the organ is enlarged in size and reacts painfully to touch; During the examination, the doctor will evaluate the nature of the discharge: its color, smell, consistency, quantity;
2. take smears – it is thanks to the simple taking of smears that the most of all pathogens of endometritis; will take the material for sowing - in this way you can study in more detail the nature of the pathogen by growing it on a special nutrient medium, as well as determine the degree of its response to a particular medical drug;
3. will take your blood for clinical and biochemical analysis(as a rule, already in a clinical blood test there will be a sufficient number of indicators to confirm the diagnosis - leukocytosis, a shift of the leukocyte formula to the left, acceleration of ESR are detected in the blood.);
4. Do an ultrasound of the uterus if possible (if you come in with already “developed” metroendometritis, in some hospitals the examination may be postponed). The main ultrasound signs of endometritis will be: thickening of the uterine mucosa, possibly blood clots and pus (in cases complicated by hemato- and pyometra), remnants of placental tissue, changes in the echogenicity of myometrial tissue during metroendometritis. Often the inflammatory process affects the fallopian tubes and ovaries, which is also clearly visible on ultrasound. In chronic endometritis, in addition to unevenly thickened endometrium, myometrium with altered echogenicity, adhesions in the uterine cavity can also be detected, which, in turn, can become the real reason infertility.
The diagnosis of chronic endometritis can be difficult, since the symptoms will be similar to many diseases of the female genital area. In this case, constant sowing of the same flora, as well as constant low-grade inflammation, will be indicative.
Treatment of endometritis
When early diagnosis Endometritis can be treated on an outpatient basis, but under the constant supervision of an obstetrician-gynecologist. Typically, treatment will consist of antipyretics and a combination of antibacterial drugs.
Treatment of acute endometritis
Unfortunately, the vast majority of women go to the doctor quite late, which leads to hospitalization and long-term treatment. In this case, you should study in detail the patient’s condition and the level of prevalence of the process and the reasons that caused it. Most often, treatment begins with:
1. intravenous antibiotic therapy: cephalosporins in combination with metragil and intramuscular gentamicin. Treatment can last from 5 to 10 days, depending on the need (cephalosporins are often replaced with aminoglycosides);
2. if there are “residues” in the uterine cavity - parts of the fetus during an incomplete abortion, the remains of the placenta after childbirth and cesarean section, curettage of the uterine cavity after infusion (intravenous drip) therapy with antibiotics is indicated;
3. use of vitamin therapy and immunomodulators;
4. application of physiotherapeutic treatment.
Treatment of chronic endometritis
Treatment of chronic endometritis is based on the effect on a specific pathogen. To do this, again, it is absolutely necessary to take smears for culture and susceptibility to antibiotics. Both an antibacterial treatment regimen (as in acute endometritis) and antiviral drugs are used.
A high therapeutic effect has been achieved by administering medications, including antibiotics, directly into the uterine mucosa. The method ensures the creation of a high concentration of medicinal substances in the lesion chronic inflammation.
In addition to this, be sure to:
1. separation of adhesions surgically (preferably hysteroscopy)
2. hormonal therapy, most often oral contraceptives, in women who want to become pregnant in the future.
Physiotherapy is widely used in the treatment of both acute and chronic endometritis in the phase when the first, most difficult period has passed and the woman is compensated. Mandatory in a hospital setting. Physiotherapeutic methods include: low-intensity UHF therapy (exposure to an ultra-high-frequency electromagnetic field) with a wavelength of 1-10 m; infrared laser therapy, etc. First of all, this makes it possible to achieve: improved outflow of fluid and pus accumulated in the uterine cavity and helps to strengthen local reparative functions.
Postpartum endometritis
A special place is occupied by postpartum endometritis, as a frequent and dangerous complication of the postpartum process. As a rule, it is inseparable from metroendometritis, is acute and makes itself felt quite early.
The main reasons are the remains of placental tissue and infection due to non-compliance with sanitary standards.
Treatment is inpatient. It consists of massive antibacterial therapy, and when the process subsides, removal of all remnants from the uterine cavity. Unfortunately, it is not uncommon for there to be complications leading to septic complications, and in this case the prognosis may be unfavorable - surgical intervention (amputation of the uterus may be necessary).
If breastfeeding, exclude breast-feeding during antibiotic therapy and for a week or two after it.
Strict adherence to a diet outside the hospital is not required. Enough: limiting fatty foods, drinking plenty of liquids, eating fruit. In case of inpatient treatment, bed rest and a diet excluding fatty and hard-to-digest foods are mandatory.
As a rule, acute endometritis with timely treatment does not require any special rehabilitation. After treatment, you need to remain under the supervision of a doctor for some time. It is possible to use physiotherapeutic procedures: radon, hydrogen sulfide and air baths, under the supervision of a physiotherapist.
Complications of endometritis
The most dangerous complications of endometritis include the spread of infection: hematogenously - through the blood; lymphogenic - lymph; along the ascending - through the fallopian tubes and descending - the cervix, vagina. This leads to “blood poisoning” - sepsis. Other complications include:
Chronization and outcome in chronic endometritis;
formation of pyometra - accumulation of pus in the uterine cavity, due to occlusion (obstruction of the cervix and the inability of pus to come out);
joining the fallopian tubes and appendages to the process – salpingitis and oophoritis;
pelvioperitonitis - as a result of pus entering the pelvic cavity.
Late complications that occur with inadequate treatment include:
Menstrual irregularities;
infertility;
constant pain in the lower abdomen.
The list of complications does not end there, since the inflammatory process can be the cause of any pathology that may emerge later. Therefore, early presentation and adequate treatment play a significant role in preventing the development of severe complications.
Folk remedies for treating endometritis
It is imperative to touch upon the population’s craze for self-medication. folk remedies. Endometritis is an inflammatory disease that can lead to extreme severe consequences. Its treatment is the responsibility of qualified obstetrician-gynecologists. Treatment should be carried out using all the latest available means to achieve maximum effect in short time. It was mentioned above that endometritis and metroendometritis are very common in the postpartum period. As evidence of the seriousness of the pathology, the following figures can be cited: from the 17th century to the beginning of the 20th century, the scourge of all maternity hospitals around the world was childbirth (or puerperal) fever - endometritis, successively turning into metroendometritis and sepsis, sometimes claiming up to 50% of lives! all postpartum women. Any experiments with folk remedies for self-medication can end disastrously for the patient.
Prevention of endometritis
Measures to prevent endometritis include eliminating factors that predispose to the occurrence of an inflammatory disease. Timely treatment of sexually transmitted infections and all complications that arise during childbirth, refusal of abortion is the most the right way prevention of endometritis.
In addition, earlier breastfeeding and the administration of contractile and immunomodulatory drugs can also serve as means of nonspecific prevention.
It is mandatory to examine the woman after childbirth, perform ultrasound and gynecological examinations.
However, the biggest preventive measure Only a woman’s attentive attitude towards herself and timely contact with a qualified obstetrician-gynecologist can help.
home
Endometritis is a pathology of the upper layers of the endometrium in the uterine cavity, manifested by inflammatory processes. Infection occurs as a result of infection of the uterus or fallopian tubes by various pathogens.
The symptoms of acute endometritis are quite unpleasant, and failure to provide timely treatment leads to a chronic form of the disease. The chronic form has less noticeable symptoms that are easily confused with other gynecological lesions. But, despite the fact that chronic endometritis does not have acute symptoms, it continues to have an extremely negative effect on the condition of the uterus and other genital organs.
Detect and treat promptly All symptoms of the disease can be achieved by regularly visiting a gynecologist.
You can recognize the disease yourself if you pay attention in time to some symptoms characteristic of this disease.
Symptoms of various forms of the disease
In total, there are two main types of endometritis: acute and chronic. Despite the fact that the chronic form is a continuation of the untreated acute form, their treatment is radically different. The most competent scheme can only be established by a specialist, after carrying out all the necessary examinations.
The acute form of the disease is the most difficult phase of endometritis, has severe symptoms and has an extremely negative effect on general state patients. The cause of poor health is the active proliferation of harmful bacteria, infection with which most often occurs during labor or during other gynecological operations. It is also worth noting that the risk of infection is much higher during a cesarean section, while during natural childbirth the incidence of infection is not so high.
The acute phase has the following symptoms:
- The following main symptoms can be identified:
- febrile conditions accompanied by chills and fever;
- uterine bleeding;
- atypical vaginal discharge (mixed with blood, pus, having an unpleasant odor and consistency);
- severe pain in the lower abdomen, spreading to the lumbar region;
- nausea and other symptoms of intoxication are possible;
- general deterioration of health.
Failure to provide timely treatment for acute endometritis provokes a serious complication in the form of a purulent form of the disease.
The manifestations of purulent endometritis are the same as those of acute endometritis, but they are supplemented by abundant purulent vaginal discharge and fever. In case of delayed discharge in the uterine cavity, pyometra may appear, which significantly aggravates the course of the disease and complicates its treatment.
In the chronic form, the following symptoms become most obvious:
- intercyclic bleeding;
- regular nagging pain in the lower abdomen;
- longer and more abundant menstruation or, on the contrary, their cessation;
- inability to get pregnant for a long time;
- regular miscarriages;
- constant subfebrile body temperature (37.1-37.8).
Often there is also increased fatigue, weakness, disturbances in the psycho-emotional state, hormonal disruptions, pain during sexual intercourse and defecation.
Prolonged inflammatory process provokes the spread of infection to the muscular layer of the uterus, which additionally leads to the appearance of a disease such as endomyometritis.
Reasons for appearance
The main cause of the development of this disease is pathogenic microorganisms. These include many bacteria, fungi and viruses, for example:
- Proteus;
- streptococcus;
- staphylococcus;
- chlamydia and mycoplasma;
- coli;
- gonococcus;
- yeast-like fungi;
- Klebsiella;
- Trichomonas;
- tuberculosis bacteria and others.
 A small probability of infection is possible in case of a decrease in the body's defenses and in case of mechanical damage to the tissues of the uterine cavity or endometrium.
A small probability of infection is possible in case of a decrease in the body's defenses and in case of mechanical damage to the tissues of the uterine cavity or endometrium.
Factors that contribute to the appearance of endometritis:
- complications during the birth process: C-section, weakness of pushing or labor, bleeding, etc.;
- installation of an intrauterine device;
- abortions and possible complications after it (remains of the fertilized egg);
- gynecological procedures (probing of the uterus, curettage, hysteroscopy);
- improperly performed douching;
- insufficient personal hygiene;
- unprotected sexual intercourse during menstruation.
Chronic form of endometritis is almost always a consequence of an untreated acute phase of the disease.
Diagnosis of the disease
The most reliable diagnostic method, especially of the chronic type, when the patient does not have pronounced complaints, is ultrasound.
- Before performing an ultrasound, a specialist conducts a survey and examination on a gynecological chair in order to establish a complete clinical picture. During examination, the uterus and appendages must be palpated to identify compactions and enlargements. The chronic form of endometritis involves deviations from the norm in the size of the uterus and its displacement. The examination also allows you to assess the nature of the discharge, its quantity, structure and color.
- A smear to determine the microflora of the vagina and cervical canal allows you to identify the presence of pathogenic bacteria and the extent of their spread. Conducting a bacteriological culture helps to identify the main pathogen that caused the symptoms of the disease. In addition, these studies may show the presence of some kind of sexually transmitted infections, for example: cytomegalovirus, mycoplasmosis, chlamydia.
- A general blood and urine test can reveal increased level ESR, leukocyte count, and changes in the leukocyte formula. Chronic endometritis also involves a decrease in platelet levels and a possible decrease in hemoglobin in the blood (anemia). These indicators indicate a blood clotting disorder, which makes any surgical procedure dangerous.
- A pelvic ultrasound allows a specialist to visually assess the size of the appendages and uterus. The presence of purulent or blood clots, synechiae, and remnants of the fertilized egg in the internal cavity is also determined. Ultrasound examination of the uterus makes it possible to establish indicators such as the thickness of the endometrium and its correspondence to the phase of the menstrual cycle.
- Hysteroscopy is an examination of the inner layers of the uterus using special equipment. Most often, such an examination is prescribed when a chronic form is suspected. Simultaneously with the examination, endometrial tissue necessary for histological examination can be collected.
How to cure
Acute form
Treatment of acute endometritis is based on the mandatory use of broad-spectrum antibiotics. They are often prescribed in combination with anti-inflammatory and painkillers. Additionally, probiotics can be prescribed to normalize the functioning of the intestinal microflora. In case of hormonal imbalances, it is recommended to take corticosteroid drugs, which improve the functioning of the ovaries and normalize the menstrual cycle.
Chronic form
Treatment of chronic endometritis should be comprehensive. Therapy for this type of disease is based on taking the necessary medications, which include:
- antibiotics;
- antimicrobials;
- immunomodulators;
- antioxidant and metabolic agents.
For greater effectiveness, the symptoms of the disease can be additionally treated with physiotherapy and folk remedies. The main criteria for the treatment of chronic endometritis are the ability to restore the microflora of the tissues of the uterine cavity, cure inflammatory processes, restore reproductive functions, normalize the cycle, and eliminate pain.
Traditional methods and physiotherapy
In order to effectively use folk remedies with endometritis, it is necessary to know exactly the causes of the disease, and also take into account individual indications and contraindications, which only the attending physician can inform you about.
In addition to application herbal infusions, which can be used in the form of tinctures, douching solutions, baths and tampons, some methods of physiotherapy can also be beneficial.
- Physiotherapy. It is very useful both as a disease prevention and during the treatment of a chronic form. A properly selected course of exercises accelerates the process of resorption of adhesions, activates blood circulation and strengthens the immune system. The result can be seen after just a month of regular exercise.
- Healthy diet. With its help, you can saturate the body with iron necessary for good health, the deficiency of which appears as a result of prolonged bleeding during illness. With this diet, the diet should be enriched with meat products, vegetables and fruits with a high iron content, as well as a decoction of rose hips.
- Vitamin therapy. Complex useful vitamins strengthens the body's immune system, accelerates metabolic processes, and activates the body's protective functions.
Treatment regimen
Most effective in modern treatment The following scheme is considered chronic:
- Stage 1 - elimination of the inflammatory process;
- Stage 2 - drug therapy aimed at restoring endometrial tissue;
- Stage 3 - elimination of hormonal imbalances and reproductive functions;
- Stage 4 - preventive measures to extend the period of remission.
Throughout the entire period necessary conservative therapy, the complex can be supplemented folk ways and physiotherapy.
Treatment with folk remedies
Most useful herbs for making therapeutic mixtures that help treat endometritis:
- chamomile flowers;
- pine buds;
- motherwort;
- dried blueberry leaves;
- tansy flowers;
- eucalyptus leaves;
- Oak bark;
- stinging nettle leaves;
- coltsfoot;
- sweet clover flowers, etc.
When using folk remedies The exact dosage of the components, as well as the methods of their application, should be taken into account.
A herbalist or herbalist will help you choose the most effective decoction.

Endometritis can also be cured using a method such as hirudotherapy (treatment with leeches). They should be applied to certain places at least 1-2 times a week, such points include:
- 4 points located directly on the stomach;
- 2 in the inguinal folds;
- 3 at the apex of the coccyx and on the sacrum;
- 1 between the 2nd and 3rd lumbar vertebrae.
The procedure is carried out exclusively by a specialist and specially prepared leeches. Leeches are used only once, so the risk of any infection is completely eliminated.

Mud treatment. This method can be treated in combination with the main therapy or used as a preventive measure for the disease. To do this you will need:
- 3 kg of special healing mud;
- 2 tablespoons of calendula flowers;
- 1 glass clean water, for boiling herbal infusion.
After brewing calendula flowers for 10-15 minutes, the decoction should be infused and strained. Mix it with mud and use it externally.
Homeopathy also refers to folk remedies and is perfect for treating chronic endometritis comprehensively. The main herbs that are used in homeopathy for this disease are:
- Kalium bichromicum;
- secale cornutum;
- belladonna;
- hydrastis;
- aurum mu-riaticum natronatum.
It is important to remember that the chronic form of endometritis is practically impossible to completely cure. Therefore, it is extremely important during the period of remission to regularly visit a specialist and follow all his instructions.
Endometritis, along with salpingitis and oophoritis, is included in the series inflammatory diseases organs of the female genital area and is rightfully considered a serious pathology. This disease occurs quite often in women of childbearing age (about 95% of all cases of the disease fall into this category).
The share of acute endometritis is 2.1% among total number gynecological diseases, while chronic endometritis is an average of 14%. The disease, especially its chronic form, poses a serious threat to women's health up to the development of infertility. The most common diagnosis is postpartum endometritis. It is observed in 5–20% of cases after spontaneous childbirth, and in 40% after abdominal delivery (cesarean section).
Endometritis – what is it?
To understand what kind of disease endometritis is, you should remember the anatomy, and in particular, the structure of the uterus.
As you know, the uterus has 3 layers. The inner layer is represented by the mucous membrane or endometrium, the middle layer, also known as the muscle layer, is called the myometrium, and on the outside the uterus is covered with a visceral layer of the peritoneum and forms the third layer - the perimeter. With regard to the development of endometritis, the inner layer is important. It consists of 2 parts: the superficial or functional layer, which is shed during each menstruation, and the basal or germinal layer, from which a new functional layer grows during each menstrual cycle. If pregnancy occurs, the functional layer hypertrophies and forms the decidua, ensuring the further development of the fertilized egg. With endometritis, the lining of the uterus becomes inflamed, specifically its basal layer (since the functional layer is renewed every month).
But speaking about endometritis, we must not forget about the more severe form of the disease - metroendometritis or endomyometritis. Since the uterine mucosa and its muscular layer are closely interconnected, inflammation of the endometrium often leads to inflammation of the myometrium, which leads to the development of metroendometritis.
From the above it follows that for endometritis to develop, a trigger factor is needed, that is, the penetration of infectious agents into the uterine cavity. Often this occurs against the background of damaged uterine mucosa, but another option is possible when the endometrium is not damaged, but the infectious agents are too aggressive.
The infection enters the uterus either through the ascending route (from the cervical canal and vagina) or through the descending route (from the uterine appendages).
Causes
As already indicated, infectious agents often enter the uterine cavity from the underlying cervix and vagina. To do this, you need 2 conditions: an open cervical canal and damaged uterine mucosa. When the integrity of the endometrium is intact, weakened immunity plays a role in the development of the disease. Therefore, a number of factors predispose to the occurrence of endometritis.
Predisposing factors
Inflammation in the uterine mucosa can be provoked by:
Induced abortion or diagnostic curettage
The development of pathology occurs either when the rules of asepsis are violated during the operation (non-sterile instruments, poor-quality treatment of the genital tract with antiseptics, etc.), or when the entire functional layer is completely removed. In the latter case, a huge wound surface is formed in the uterus, which is easily attacked by pathogenic microorganisms.
Spontaneous termination of pregnancy
In this case, the occurrence of complications is facilitated by the remains of the fertilized egg, which are an excellent breeding ground for microorganisms and, even if they remain in the uterine cavity for a short time, provoke the development of pathology.
Hysteroscopy or hysterosalpingography
In addition to the expansion of the cervical canal during these procedures, weakened immunity and disruption of the integrity of the endometrium play a role.
Insertion of an intrauterine device
The infection enters the uterus through the threads of the intrauterine contraceptive device or if the rules of asepsis for inserting the device are not followed or if the woman’s examination is not carried out (smear tests).
Douching
Frequent and unreasonable douching disrupts the normal microbiocenosis of the vagina, which leads to a decrease in the protective properties of the vagina and cervix and allows the free penetration of pathogenic microbes into the uterine cavity.
Prolonged labor
Labor that lasts more than 12 hours usually occurs against the background of an open amniotic sac. The uterine cavity becomes accessible for infection to penetrate and multiply in it, which is accompanied not only by the occurrence of postpartum endometritis, but is also fraught with danger for the baby.
Sexual intercourse during menstruation
During menstruation, the cervix opens slightly, and the functional layer is torn away, exposing the germinal layer of the endometrium. Unprotected sexual intercourse during this period contributes to the penetration of infection into the “open wound” in the uterus and the occurrence of pathology.
Other reasons
- Probing of the uterus- penetration of infection into the uterine cavity through a probe.
- Manual separation of the placenta— endometritis often develops after intrauterine interventions during childbirth (manual separation of the placenta or manual control of the uterine cavity).
- Weakened immunity- contributes to decreased immunity long-term use hormonal drugs, antibiotic therapy, recent infectious diseases, HIV infection.
- IVF and artificial insemination.
Pathogens of endometritis
The causes of endometritis are microorganisms. These can be bacteria, viruses, protozoa or fungi. But the disease is rarely caused by one type of microbe; as a rule, its occurrence is facilitated by an association of infectious pathogens.
Bacterial endometritis is caused by:
- gonococcus;
- streptococcus;
- coli;
- Koch's bacillus (the causative agent of tuberculosis);
- Klebsiella;
- Proteus;
- causative agent of diphtheria;
- chlamydia;
- mycoplasma;
- enterobacter.
Viral endometritis is caused by:
- cytomegalovirus;
- herpes simplex virus;
- human papillomavirus and others.
Fungal endometritis is caused by fungi of the genus Candida. Trichomonas are among the protozoa that cause the disease.
Classification
Depending on the course of the disease, there are:
- acute endometritis;
- subacute process;
- chronic illness.
Depending on the severity of clinical manifestations, the degrees of the disease are distinguished:
- mild course;
- moderate;
- severe degree.
Depending on the infectious agent, endometritis is divided into:
- specific (Trichomonas, gonococci, Mycobacterium tuberculosis and others);
- nonspecific endometritis caused by opportunistic microorganisms.
According to the results of histology (pathomorphological forms);
- atrophic – characterized by atrophy of the glands and fibrosis of the stroma, infiltration of the latter with leukocytes;
- cystic - with stromal fibrosis, compression of the gland ducts occurs, which leads to stagnation and thickening of their contents and the formation of cysts;
- hypertrophic – characterized by excessive growth of the endometrium, which requires therapeutic curettage of the uterine cavity.
Such forms of the disease as catarrhal endometritis, as well as purulent catarrhal endometritis, are not used in the “human” classification; this applies to the division of the disease in animals (cows, dogs, cats).
Clinical picture
The symptoms of the disease depend on many factors:
- aggressiveness of the pathogen;
- state of immunity;
- patient's age;
- predisposing conditions (endometritis occurs especially severely against the background of an IUD, after a miscarriage or complicated childbirth);
- area of damage to the uterine mucosa;
- the presence of concomitant gynecological pathology.
Acute endometritis
The incubation period for acute endometritis is 3–4 days. Clinical picture postpartum endometritis develops no later than the 4th day. The larger the area of the uterine mucosa that becomes infected, the more pronounced the symptoms and the more severe the course of the disease. The main signs of an acute process include:
Intoxication
First of all, this is manifested by a significant increase in temperature (39 - 40 degrees), accompanied by chills and increased sweating. On the background high temperature other signs of intoxication appear: weakness, lethargy, loss of strength, loss or decrease in appetite, nausea and even vomiting.
Pain
Pain in the lower abdomen can be of various types, from aching to unbearable. Sometimes the pain is localized in the lumbar or sacral regions, often radiating to the legs, under the shoulder blades. Patients often indicate the characteristic localization of pain - above the pubis in the middle part lower section belly. With severe inflammation, the pain syndrome may be accompanied by peritoneal symptoms (Shchetkin-Blumberg sign and others).
Discharge
Perhaps the most characteristic sign of this disease. Mucopurulent or purulent and profuse discharge is noted, which is accompanied by an unpleasant odor (mainly with purulent endometritis caused by pyogenic bacteria). Due to desquamation (rejection) of the mucous membrane and the slowdown in its recovery, the discharge may be mixed with blood, which is called “the color of meat slop” or sanguineous and lasts for quite a long time.
In total, purulent endometritis is nothing more than pyometra, when it accumulates in the uterus a large number of pus, and the cervical canal is closed or slightly open. Pyometra is most typical for spontaneous and criminal abortions.
Chronic endometritis
In the absence or in case of incomplete treatment, the process becomes chronic, which is fraught with many complications. The signs characteristic of the acute process are somewhat smoothed out, so it is difficult to diagnose the chronic course of the disease. Symptoms of chronic endometritis include:
Temperature
Patients note a constant increase in temperature to insignificant numbers (not higher than 38), against the background of which there is a feeling of weakness and weakness, decreased performance and increased fatigue.
Cycle disorders
To others characteristic features Chronic endometritis includes various cycle disorders. This may manifest as elongation and increase in volume. menstrual flow(hyperpolymenorrhea), irregular uterine bleeding (metrorrhagia), spotting before and after menstruation. Such violations are associated, firstly, with growths connective tissue(fibrosis), which disrupts the cyclic processes in the endometrium (proliferation and rejection). Secondly, this is due to a violation of the contractile function of the uterus. And, thirdly, with a violation of platelet aggregation, which leads to its prolongation instead of stopping the bleeding.
Pain
Patients often complain of constant pain in the lower abdomen and/or lower back of slight intensity or discomfort. Pain during bowel movements and sexual intercourse is also typical.
Discharge
The chronic process is almost always accompanied by copious mucous or mucopurulent discharge, often with a putrid odor.
Reproductive disorders
For chronic disease Miscarriages or infertility become common.
Is pregnancy possible?
Despite the seriousness of the disease, endometritis does not exclude the possibility of conception and subsequent progression of pregnancy. Undoubtedly, in many cases of a chronic process, pregnancy becomes a pipe dream, but with desire and some effort, this dream can not only be brought closer, but also realized.
Chronization of the process leads to a decrease in the area of the normal, that is, healthy endometrium, which is necessary for the implantation of a fertilized egg and its support in further development. After all, it is the normally functioning uterine mucosa that is capable of growing by the end of the 2nd phase of the cycle, that is, preparing the so-called “featherbed” for receiving the future embryo and, after the implantation of the zygote, providing it with all the necessary nutrients in the initial stages of development.
Chronic endometritis does not exclude the possibility of fertilization (with existing ovulation), but pregnancy (in this case we're talking about O biochemical pregnancy, when fertilization has occurred, but implantation has not yet occurred) is interrupted at the stage of implantation of the zygote into the uterine mucosa. Most women do not even suspect that they have had a miscarriage at very early, clinically it looks like a slightly late menstruation.
But even with successful implantation, pregnancy is often interrupted in the first trimester, and miscarriages regularly recur (recurrent miscarriage). If, despite everything, the pregnancy continues to develop, then the process itself is accompanied by numerous complications, from the permanent threat of miscarriage to the birth of a child with growth retardation until his death (during pregnancy, during childbirth or shortly after).
In the case of an acute process, there is no point in talking about pregnancy until adequate treatment has been completed. But is it possible to get pregnant with chronic endometritis? In order not to scare women right away, the answer is positive: “yes, pregnancy is quite possible.” But what is needed for this?
Firstly, approach pregnancy consciously, which means thinking about the problem at the planning stage. It is necessary to visit a gynecologist and related specialists according to indications, start leading a healthy lifestyle, refuse bad habits(this also applies to your spouse), take vitamins and get examined. The minimum examination includes gynecological smears, pelvic ultrasound, tests for hidden sexually transmitted infections, and in some cases, hormone tests.
If the diagnosis of chronic endometritis is confirmed, and especially if hidden sexually transmitted infections are detected, the gynecologist will prescribe treatment. The therapeutic course is very long, but it is important to complete it to the end. First of all, antibiotics are prescribed depending on the sensitivity of the isolated pathogen. At the second stage of endometritis treatment, physiotherapy, immunomodulators, vitamins, proteolytic drugs, and in some cases oral contraceptives are included. Hormonal contraceptives are necessary to restore the cyclic change of the functional layer of the endometrium.
After successful treatment of endometritis future mom She undergoes an examination again, in particular a pelvic ultrasound, at which she is confirmed to have inactive endometritis when the disease is in remission, and is given the go-ahead to try to get pregnant.
Diagnostics
Diagnosis of endometritis should include:
- Collection of anamnesis and complaints
- Gynecological examination
Bimanual palpation reveals a slightly enlarged and softened uterus, painful when palpated. Displacement behind the cervix and palpation of the vaginal vaults are also painful, which indirectly confirms the involvement of the uterine appendages in the process.
Signs of inflammation are detected in the peripheral blood: accelerated ESR, leukocytosis with a shift to the left, anemia is possible.
- Gynecological smears
Examination of the contents of the vagina and cervical canal in most cases allows us to identify the causative agents of the disease.
- Tank. culture of secretions
The tank is being carried out. culture of vaginal and cervical secretions for more accurate identification of the pathogen and determination of its sensitivity to antibiotics.
- PCR diagnostics
Allows you to identify hidden sexually transmitted infections.
Ultrasound of the pelvic organs confirms the diagnosis and excludes complications. But in the case of a chronic process, ultrasound data is not enough to confirm the diagnosis.
- Hysteroscopy followed by diagnostic curettage of the uterus
Hysteroscopy allows you to visually assess the condition of the uterine walls, and the material obtained during curettage confirms the diagnosis histologically. The procedure is prescribed if a chronic course of the disease is suspected.
Treatment
The tactics of treating endometritis in women is determined by its course, the severity of the process, the pathogens cultured and concomitant pathology. As a rule, therapy for an acute process or during exacerbation of a chronic process is carried out in a hospital.
For acute endometritis
- Basic therapy
First of all, the patient is hospitalized. Immediately upon admission, she is prescribed bed rest and cold applied to the lower abdomen (stimulates the contractile activity of the uterus, reduces pain, and has a hemostatic effect). Drinking plenty of fluids (to relieve intoxication symptoms) and an easily digestible diet rich in vitamins and protein are prescribed.
- Surgery
Surgical treatment is carried out according to indications. If pathology develops against the background of an intrauterine contraceptive, its immediate removal is carried out. If the cause of the disease is the remains of the fertilized egg after a miscarriage or medical abortion, or the remains of the placenta after childbirth (independent or surgical), immediate emptying of the uterine cavity (curettage) is required.
Curettage of the uterine cavity is performed only after massive infusion therapy with saline solutions and a decrease in temperature (to 37.5, at least to 38 degrees).
- Antibiotic therapy
Antibiotics take first place in the treatment of disease. At acute process antibacterial drugs are prescribed systemic action(intramuscular or intravenous). Considering that this pathology is often caused by an association of microbes, the treatment regimen for endometritis is combined and, in addition to broad-spectrum antibiotics, includes metronidazole preparations (active against anaerobes):
- cephalosporins 3 – 4 generations intramuscularly + metrogyl intravenously;
- lincosamides + aminoglycosides 2 – 3 generations intramuscularly;
- clindamycin + chloramphenicol intramuscularly;
- gentamicin + chloramphenicol intramuscularly;
- lincomycin + clindamycin intramuscularly.
Antibacterial therapy is prescribed until the results are obtained. sowing smears and determining pathogens and their susceptibility to prescribed drugs, since the results of the analysis become known no earlier than after 7 days, and treatment should begin immediately. Depending on the results, the previously started treatment is continued or the necessary drug is added. The general course of antibiotic therapy is 7–10 days.
- Infusion therapy
Salt solutions (glucose solution with ascorbic acid, saline solution with B vitamins, Ringer's solution and others) and colloidal solutions (reopolyglucin, infucol, hemodez) are administered intravenously for detoxification purposes. The total volume of administered solutions should be at least 2000 - 2500 ml daily.
- Other drugs for endometritis
At the same time, antihistamines (suprastin, clarotadine, tavegil and others), antifungals (oral flucostat), immunomodulators (viferon), vitamins and probiotics are prescribed to restore normal vaginal microflora.
For chronic endometritis
How to treat chronic endometritis? Therapy for a chronic disease is carried out comprehensively, in several stages and on an outpatient basis (except for exacerbations).
- Antimicrobial therapy
After examination using the PCR method, drugs are specifically prescribed depending on the isolated pathogen. For example, when chlamydia and mycoplasmas are detected, doxycycline is prescribed, for a viral infection, acyclovir, for a fungal etiology, flucostat, orungal systemically.
- Uterine lavage (intrauterine dialysis)
Diffuse washing of the uterine cavity with antibacterial and antiseptic drugs creates a high concentration of the drug in the focus of chronic inflammation. For lavage of the uterus, anti-inflammatory solutions (furacillin, chlorhexidine, dimexide, dioxidine), anesthetic solutions (novocaine, calendula tincture) and solutions and enzymes that prevent the formation of intrauterine adhesions (lidaza, longidase) are used. The course of washing is 3 – 5 procedures, the volume of liquid per procedure reaches 2.5 – 3 liters (until the washing liquid is completely clarified). The procedure lasts 1 – 1.5 hours. Washing is carried out with cooled solutions (4 - 5 degrees), which creates a hypothermic effect, relieves pain and stimulates uterine contractions. In the presence of bloody discharge from the uterus into the lavage include aminocaproic acid (hemostatic effect).
- Suppositories for endometritis
Suppositories with an antibacterial component are selected depending on the pathogen isolated (polygynax, betadine, clotrimazole). Suppositories with a proteolytic effect are prescribed to prevent the formation of adhesions in the uterus and pelvis (longidaza, propolis). Suppositories with indomethacin, diclofenac, voltaren (introduced into the rectum) are prescribed as an analgesic and anti-inflammatory agent.
- Metabolic drugs
As remedies for chronic endometritis, drugs with metabolic activity (Actovegin, vitreous, aloe extract) are used, which promote endometrial regeneration processes and stimulate local immunity. Intravaginal administration of tampons with sea buckthorn oil and honey is also recommended.
- Hormone therapy
Cyclic hormonal drugs (COCs) are prescribed to patients of childbearing age in order to restore the cyclic change of the endometrium in the cycle, eliminate intermenstrual bleeding, and normalize the duration and volume of menstrual flow. Monophasic drugs are prescribed (rigevidon, novinet, regulon).
- Enzymes and multivitamins
- Immunomodulators
Prescribed to increase general and local immunity and create a favorable immune background necessary for successful implantation (Wobenzym, Thymalin, Taktivin, Likopid, Viferon, Immunal)
- Physiotherapy
A long-term and effective stage of treatment for both endometritis and other diseases of the uterus.
Physiotherapy relieves inflammatory swelling of the uterine mucosa, activates blood circulation in the pelvis, stimulates local immunity and endometrial regeneration. Among the effective physiotherapy procedures are UHF, electrophoresis of zinc and copper by cycle phases, electrophoresis with lidase and iodine, ultrasound and magnetic therapy.
- Spa treatment
During the rehabilitation period, patients with a chronic process are recommended to visit sanatoriums for courses of mud therapy and balneotherapy.
Question answer
What are the dangers of acute and chronic endometritis?
The acute course of the disease if not consulted in a timely manner can lead to the development of pyometra, when the uterine cavity is filled with pus, salpingo-oophoritis, pelvioperitonitis, and in advanced cases to sepsis and even the death of the woman. With an untreated acute process, endometritis becomes chronic, which in turn is fraught with the formation of adhesions in the uterine cavity and pelvis, chronic pain, cycle disruption, infertility and recurrent miscarriage.
What is the prevention of endometritis?
There is no specific prevention of the disease. You should only be attentive to your own health: exclude casual sexual intercourse or use a condom, undergo timely preventive examinations, if hidden sexually transmitted infections are detected, follow all doctor’s recommendations, refuse abortions, and observe the rules of intimate hygiene.
Are endometritis and endometriosis the same thing?
No, these are completely different diseases. Endometritis (the ending “it” means inflammation) is an inflammatory process in the uterine mucosa, and endometriosis is the spread of endometrioid cells, similar in structure to endometrial cells throughout the body. Endometrioid cells undergo all the cyclic changes that occur in the endometrium during the menstrual cycle. In particular, during menstruation, blood is released from endometrioid cells, which causes pain and contributes to the formation of adhesions in abdominal cavity. Endometritis is inflammation, and endometriosis is a hormonal disease.
Is it possible to have sex with endometritis?
In case of an acute process or exacerbation of a chronic one, a strict ban on sexual activity is imposed. If chronic endometritis is in remission, sex life is not prohibited, you should only use barrier methods of contraception.
Often women develop endometritis after abortions, childbirth and miscarriages. It is worth noting that endometritis can be treated quite successfully. Endometritis is an inflammation of the uterine mucosa caused by viruses and various pathogenic microorganisms: streptococci, E. coli, gonococci, staphylococci, chlamydia and trichomonas.
Causes of the disease
The endometrium of the uterus consists of two layers: basal and functional. The structure of the functional layer is quite fragile and sensitive. Damage to this structure can lead to the development of the endometrium. It is worth noting that the damage itself does not lead to serious complications; uterine endometritis is caused by viruses that penetrate through these damage.
So, endometritis can occur due to the following reasons:
- Inaccurate douching;
- Probing of the uterine cavity;
- Examination of the fallopian tubes;
- Curettage of the uterine cavity
The following pathogens also cause endometritis:
- Tuberculosis microbacteria;
- Chlamydia;
- Proteus;
- Escherichia coli;
- Diphtheria bacillus;
- Klebsiella;
- Group B streptococci;
- Mycoplasmas;
- Enterobacter
Symptoms and manifestations of endometritis
In the initial stages of the disease, the symptoms of endometritis do not appear too clearly, so a woman cannot detect endometritis in time and seek treatment.
It is worth noting that uterine endometritis can be chronic and acute. Basically, acute endometritis occurs due to mechanical damage. Chronic endometritis develops as a result of infection with sexually transmitted infections.
Symptoms of acute endometritis
In the first days after childbirth, abortion and diagnostic procedures, acute endometritis may form, the symptoms of which manifest themselves as follows:
- general deterioration of condition: headache, lack of appetite and so on;
- weak, aching or nagging pain in the lower abdomen;
- pain radiating to the sacrum or lower back;
- increase in body temperature up to 39 degrees;
- uterine bleeding;
- vaginal discharge with an unpleasant odor, resembling clots of blood and pus.
If you have signs of endometritis, you should immediately consult a doctor, since endometritis grows quite quickly and affects large areas. The longer you do not see a doctor, the more difficult it will be to cure acute endometritis.
Symptoms of chronic endometritis
Chronic endometritis, as a rule, is associated not with gynecological intervention, but with the appearance of sexually transmitted diseases. Therefore, in this case, the symptoms of endometritis will correspond to the symptoms infectious diseases. So, signs of chronic endometritis:
- weak aching pain in the lower abdomen;
- vaginal discharge corresponding to discharge during infections, for example, with gonorrhea, yellowish-green purulent diseases appear, with abundant foamy discharge;
- increase in body temperature to 37-38.5 degrees;
- heavy menstruation lasting more than 7 days;
If you find signs of endometritis, you should immediately seek qualified treatment, since chronic endometritis can cause miscarriage and infertility.
Treatment of endometritis

If uterine endometritis is detected on time, treatment can be carried out on an outpatient basis. But even if outpatient treatment of endometritis is carried out, it should be carried out under the supervision of a gynecologist. If the disease is advanced, endometritis is treated in a hospital. As a rule, endometritis is treated according to the following scheme:
- antibacterial therapy;
- antibiotic therapy;
- cleaning the uterine cavity;
- purifying the blood of toxins produced by bacteria.
Treatment of acute endometritis
If acute endometritis is diagnosed in a timely manner and treatment is started on time, then the prognosis is favorable and there will be no problems with further pregnancy. Treatment of acute endometritis is as follows:
- taking vitamins and immunomodulators;
- intravenous administration of antibiotics: cephalosporin with metragil;
- intramuscular administration of antibiotics: gentamicin;
- if endometritis is caused by the fact that after an abortion there are remains of the fetus in the uterus or after childbirth - the remains of the placenta, it is necessary to perform curettage of the uterine cavity;
- physiotherapy.
Treatment of chronic endometritis
As noted above, the symptoms of chronic endometritis differ from the symptoms of acute endometritis, and accordingly, treatment methods will also be different. If chronic endometritis is detected, smears are taken from the patient to determine the susceptibility of infections to various types of antibiotics. This will allow you to select best option treatment. Then endometritis is treated using an antibacterial regimen with the addition of antiviral drugs.
Treatment of chronic endometritis is considered more effective if medications are injected directly into the uterine mucosa, since this method makes it possible to concentrate a larger amount of drugs directly at the site of inflammation.
Additionally, chronic endometritis can be treated with:
- hormonal therapy (oral contraceptives are most often prescribed to women who are being treated for endometritis and planning a future pregnancy);
- separation of adhesions using surgical operations;
When uterine endometritis is cured, physiotherapy is prescribed, which helps to increase the outflow of mucus and pus from the uterine cavity.
Treatment of purulent endometritis
Purulent endometritis is most often treated with mechanical cleaning of dead tissue and removal of pus from the uterine cavity. Mechanical cleaning of the uterine cavity is carried out under general anesthesia. Next, hormone therapy is carried out.
Treatment with folk remedies

IN Lately Treatment with folk remedies is becoming increasingly popular in the fight against many diseases. It is worth noting that endometritis is a serious disease that requires qualified therapy, so it is necessary to consult a doctor who can make an accurate diagnosis and prescribe qualified treatment. But, if you decide to try treatment with folk remedies, we will describe several recipes that should help eliminate endometritis.
- An infusion of herbs will help cure endometritis: marshmallow root, cudweed, Leuzea, lavender, wormwood, sweet clover leaves, nettle leaves, blueberry leaves, pine buds. Herbs are mixed into equal parts and grind well. Pour 2 tablespoons of herbs into a thermos and pour 3 cups of boiling water. The infusion is infused for 12 hours, then filtered. Take 3 times a day, 1/3 cup. Endometritis is treated with this infusion for 2 months.
- Endometritis is also treated with an infusion of the following herbs: bearberry, thyme, herb, coltsfoot, calendula flowers, dandelion, chicory, bergenia root and angelica. The herbs are crushed and mixed in equal parts, then 2 tablespoons of the mixture are poured with 3 cups of boiling water. The infusion is kept for 12 hours, and then filtered and taken 1/3 cup 3 times a day. Endometritis is treated with this composition for 2 months.
- Laurel laurel can help cure endometritis. For the infusion you will need 20 grams of laurel and a bucket of water. In this case, endometritis is treated with sitz baths.
- Even if treatment with folk remedies helped, and you feel much better and the symptoms disappear, after treatment it is recommended to consult a doctor so that he can do tests and evaluate the effectiveness of the treatment. Since there is a risk that you will simply relieve the symptoms and not cure the endometritis itself, this can lead to such a serious consequence as infertility.
DOCTOR consultations online
Patient: how justified is the treatment of endometritis - antibiotics for 3 weeks + nice and physiotherapy, after 3 months hormonal pills
Doctor: In principle, absolutely justified.
****************
Patient: Hello, I was diagnosed with metroendometritis, treated with antibiotics, the pain continues, is it worth treating with herbs?
Doctor: Hello, if the course of antibiotic therapy and anti-inflammatory drugs is completed, then you can
***************
Patient: Is it possible to die from purulent endometritis?
Doctor: This condition can cause the development of sepsis, and this is truly life-threatening.